Why Building a Support System After Trauma Is Important

Experiencing trauma can be life-altering, leaving individuals feeling isolated, overwhelmed, and emotionally vulnerable. While healing from trauma is a deeply personal journey, it should not be navigated alone. Building a strong support system in Salt Lake City, Ogden, and Logan is essential in fostering recovery, promoting emotional resilience, and restoring a sense of safety and connection.
The Impact of Trauma on Mental Health
Trauma can take many forms, including physical, emotional, or psychological distress caused by events such as abuse, loss, accidents, or violence. Without proper support, trauma survivors may struggle to regain stability and find the strength to move forward. This is why building a support system is crucial.
The Benefits of a Support System
A strong support system in Salt Lake City, Ogden, and Logan provides emotional, psychological, and sometimes even physical reinforcement during healing. Some key benefits include:
1. Emotional Validation and Understanding
Having people who listen and validate your experiences helps reduce feelings of isolation. Knowing that others acknowledge your pain can be incredibly comforting whether it’s a trusted friend, therapist, or support group.
2. Encouragement and Motivation
Healing from trauma can feel overwhelming, but a support system provides encouragement to keep moving forward. Supportive individuals can help motivate you to seek therapy, engage in self-care, and adopt healthier coping strategies.
3. Reduced Feelings of Isolation
Trauma can make survivors feel disconnected from the world. Engaging with others who offer empathy and understanding can help restore a sense of belonging and prevent loneliness from taking hold.
4. Help with Practical Needs
Sometimes, trauma impacts daily functioning. A strong support system can assist with practical matters such as childcare, errands, or attending medical appointments, helping alleviate additional stressors.
5. Healthier Coping Mechanisms
Surrounding yourself with supportive individuals can encourage healthier coping strategies, reducing reliance on negative habits such as substance abuse or self-isolation. Friends, family, or professionals can guide trauma survivors toward constructive emotions management.
How to Build a Support System
Creating a reliable support network in Salt Lake City, Ogden, and Logan requires intentional effort, but it is possible even in difficult circumstances. Here are some ways to establish a strong foundation:
1. Reach Out to Trusted Individuals
Identify people who have been reliable, understanding, and nonjudgmental. This could be close friends, family members, or mentors who genuinely care about your well-being.
2. Join a Support Group
Connecting with others who have experienced similar trauma can be incredibly validating. Support groups, in-person or online, offer a sense of community and shared understanding.
3. Seek Professional Support
Therapists, counselors, and support organizations provide specialized guidance tailored to trauma recovery. Professional support can be a crucial element in the healing journey.
4. Set Boundaries with Unsupportive Individuals
Not everyone in your life can provide the support you need. It is important to establish boundaries with those who are dismissive or toxic to your healing process.
5. Engage in Community and Social Activities
Reconnecting with the world can be challenging, but joining social activities, volunteering, or engaging in hobbies can help build meaningful relationships outside of past trauma.
Seek Help with PPH
While it may feel difficult to open up or seek help, having a support system can make all the difference in rebuilding a sense of safety, trust, and hope. Surrounding yourself with people who uplift and validate your experiences can be a powerful step toward reclaiming your life and moving forward with resilience.
Contact PPH today to learn more about ways to heal from trauma. We have offices in Salt Lake City, Ogden, and Logan and look forward to meeting you.
How Does Trauma Affect The Brain?
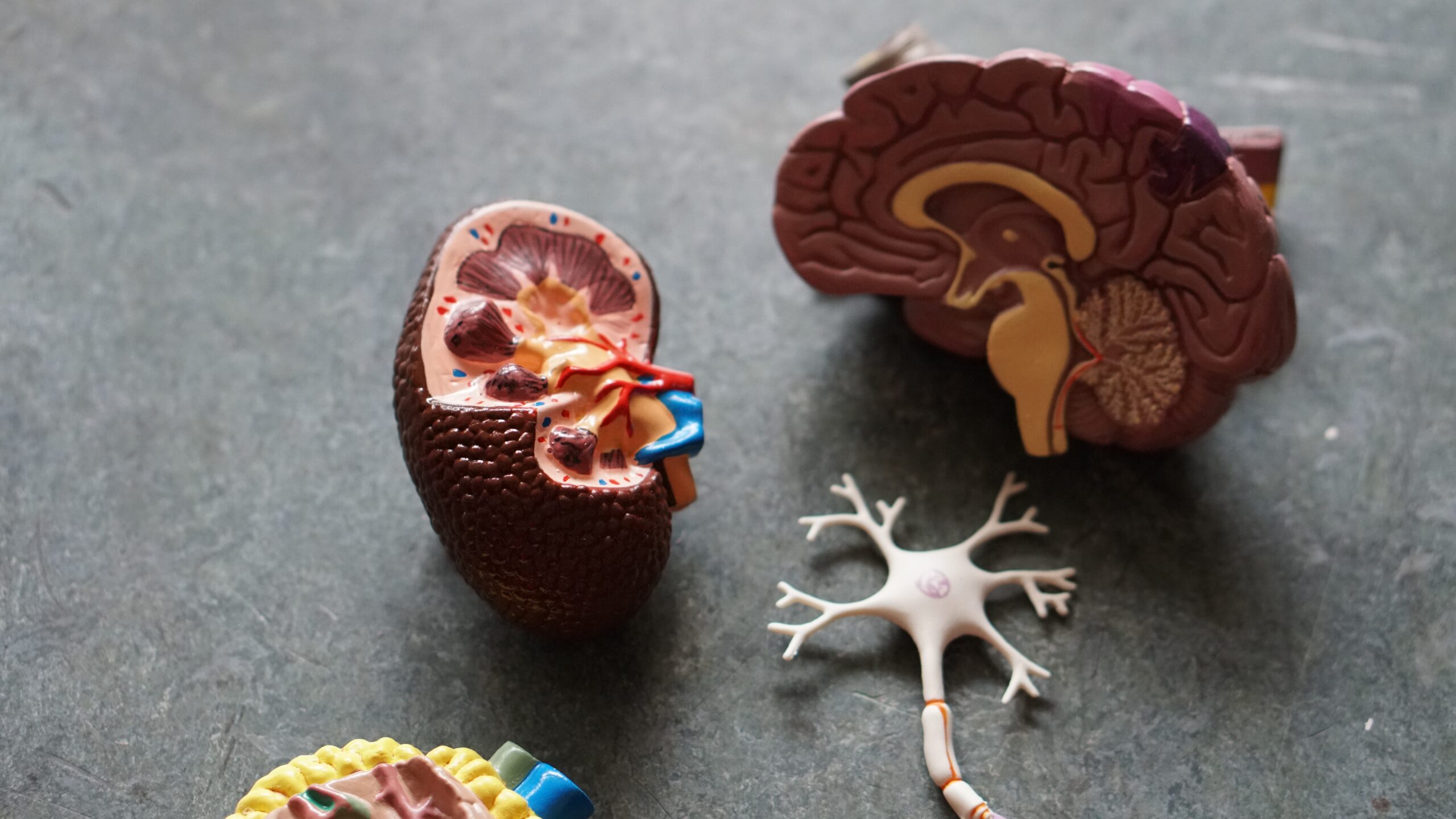
Trauma can have a profound impact on the brain, affecting both its structure and function. When an individual experiences trauma, their brain’s response mechanisms can significantly alter. This often results in heightened stress responses, with the amygdala becoming overactive, leading to increased anxiety and hypervigilance.
What is Trauma?
Trauma is an emotional response to something that has happened—like physical, emotional, or life-threatening harm.
It’s normal for most people to experience trauma; however, the main difference for people with trauma-related mental health problems is difficulty moving on with their lives.
Trauma knows no bounds—whether it is age, gender, or socioeconomic status. And as common as trauma is, many don’t realize how much it truly affects you from the inside out.
How Trauma Changes The Brain’s Chemistry
For the mind and body to function properly, the different parts of the brain need the ability to communicate. However, when a part of the brain changes due to trauma, it becomes a catalyst for other problems to arise.
The hippocampus, a critical memory and emotional regulation region, can shrink in response to chronic stress and trauma. This can impair memory formation and make it more challenging to process and cope with the emotions associated with the traumatic event.
Also, the prefrontal cortex, responsible for decision-making and impulse control, can be affected by trauma. This can result in difficulties in regulating emotions and making rational choices. Additionally, some individuals may develop dissociative symptoms, where their sense of self becomes disconnected from their surroundings, impacting brain regions related to self-awareness and perception.
Furthermore, neurotransmitter balance can be disrupted—affecting mood regulation and reward processing. These alterations contribute to symptoms of depression, anxiety, and other mood disorders. Trauma may also heighten sensory processing, increasing sensitivity and flashbacks triggered by sensory cues.
In severe trauma cases, PTSD can lead to specific brain function and structure changes. Disruptions in brain networks, such as the default mode network, may result in intrusive thoughts and a persistent sense of danger. Connectivity between brain regions involved in emotional processing and memory can also become disrupted.
Some trauma survivors may experience distortions in their perception of time, feeling as though the traumatic event is continually happening or struggling to organize past and present experiences.
The Impact of Trauma
It’s important to remember that not everyone who experiences trauma will develop lasting brain changes or mental health conditions.
Resilience, social support, and timely intervention can mitigate the long-term impact of trauma on the brain, and therapeutic approaches like cognitive-behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), and medication can help individuals cope with and recover from trauma-related brain changes and associated psychological symptoms.
If you or someone you know has experienced trauma and needs trauma therapy, contact the professionals at Psychological Preventative Health today.
34th Annual Boston International Trauma Conference | Part 4


34TH ANNUAL BOSTON INTERNATIONAL TRAUMA CONFERENCE | PART 3


34th Annual Boston International Trauma Conference (https://
34th ANNUAL BOSTON INTERNATIONAL TRAUMA CONFERENCE | Part 2


Come with me for day by day takeaways on the latest and greatest in trauma treatment:
34th Annual Boston International Trauma Conference (https://
1. Conversations about SMART Implementation Across Cultures.
Featuring Elizabeth Warner, Alexandra Cook, Anne Westcott, Heather Finn, Alicia Hu, Mei Ling Hu, Kasey Pendexter, and Mari Kjølseth Braein. (https://
SMART is a form of body focused therapy currently focused on children and teens however there are current projects exploring what this could look like for adults. SMART stands for Sensory Motor Arousal Regulation Therapy.
2. IFS and Addictions.
3. Keynote Talk: Psychological Trauma Underlying Mental Processes.
1. Conversations about SMART Implementation Across Cultures.
2. IFS and Addictions.
I have a love love relationship with IFS (Internal Family Systems). A very, very brief overview of this therapy is that all of us have a core “Self” that is considered: compassionate, curious, creative, confident, calm, clear, courageous, and connected. This “Self” is who we really are underneath different “parts” that developed in almost extreme ways to help us or the “Self” cope with something traumatic or dysfunctional. “Parts” come in three categories and those categories can have multiple different behaviors, attitudes, thoughts that come with them.
There are “exile parts” that are parts of us that have been hurt, traumatized, sad; they are exiled because our system wants to protect us from danger, discomfort, and to keep us safe. There are “manager parts” that rush in the extreme to make sure the exiles never get triggered. An example of a “manager” would be an internal critic – the critic’s job is to make sure we don’t do things that trigger the exile and that voice comes with a lot of shame typically. Then there are “firefighter parts”; these are parts that rush in when an “exile” breaks through a “manager”‘s efforts and will do anything to decrease the emotion, thought, hurt by any means. These means can be addiction, daily behaviors (shopping, distracting, avoiding), self-harm, and suicide. These “firefighters” do anything to keep us safe and safety comes to mean that our exiles don’t feel hurt anymore.
3. Keynote Talk: Psychological Trauma Underlying Mental Processes.
Gabor Mate (https://drgabormate.com) and Richard Schwartz (https://ifs-institute.com/
These two men have created a different way to consider trauma, healing, and the human experience. For me personally they have changed the way I am a therapist and the way that I relate to myself and others.
34th Annual Boston International Trauma Conference | Part 1


Come with me for day by day takeaways on the latest and greatest in trauma treatment:
34th Annual Boston International Trauma Conference (https://traumaresearchfoundation.org)
This year I am attending the conference from the comfort of my living room and home office 🙂 And…it is completely worth it! The conference this year is 4 days of amazing information from researchers and practitioners that continue to create the best treatment options for individuals living with trauma and those of us who work in the trauma field.
Today I attended “From Empathic Distress to Compassion: Building Resilience in the Face of Trauma” with Tania Singer (https://taniasinger.de) and Ronald Siegel (https://drronsiegel.com)
They discussed research that is helping to train peoples’ minds to improve three things:
- attention & mindfulness (through breathing meditations and body scans)
- care & compassion (through loving kindness meditations and dyad exercises)
- cognitive perspective taking & theory of mind (through dyad exercises and observing-thoughts meditations)
A few interesting things they brought up early on is that attention & mindfulness are self oriented skills. Care & compassion are self and other oriented skills (about relating to others and relationships). Cognitive perspective taking is a self and other oriented skill that is called “meta” meaning that you work on thinking about how you and others are thinking.
The main research study here can be found on Tania Singer’s website (https://taniasinger.de) under the menu topic ReSource Project. This study was conducted for at least a year and phases were done in person as well as virtually because part of the study occurred while Germany was in lock down d/t COVID 19. Two things she shared from this study was seeing that the brain actually thickens, grows, and shows improvements in people who were doing the training. The parts that grow play a role in empathy, care and compassion. Second thing – that peoples’ capacity and tolerance for social situations increases.
Now, for those of us living with trauma this may sound great but very overwhelming. When it comes to tools, resources, and healing therapy is still a great way to go. Finding a therapist who will work with you, be patient, listen to you and provide some gentle guidance; all good things. One timeline for healing with improving feeling and sensation in the body as well as ability to name those things was 6-9 months with help.
Okay, cutting this short here because really; this is better learned and done together. Head over to the Meet Our Team tab and see if anyone of us feel like a good fit to help you in healing from trauma and learning to find compassion for yourself.
Come back tomorrow where I will be writing about “How to incorporate Neurofeedback into Trauma Treatment – Latest Developments”; “IFS and Addictions” … and possibly more!
Written by Katie Walter



